Malaria is both preventable and treatable. Still, nearly half the world’s population is at risk of contracting the disease. Africa suffers disproportionately high rates of malaria illness and death, even after years of progress1. For instance, the entire population of Liberia is at risk of contracting malaria2, and approximately one-quarter are diagnosed with it each year3. While far fewer people died from malaria in 2016 than in 2005, it is still the country’s second leading cause of death4.
Liberia continues to face this challenge while recovering from 14 years of civil war that affected physical, economic, and governmental infrastructures. Created in 2010, Liberia’s medicines regulatory authority—the Liberia Medicines and Health Products Regulatory Authority (LMHRA)—is a critical step forward in reducing the country’s vulnerability to the proliferation of poor-quality medicines.
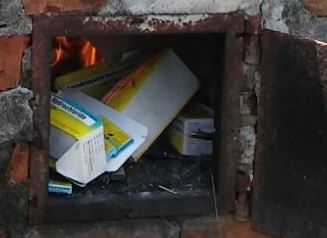
LMHRA incinerates banned, poor-quality antimalarials collected from the 17 districts of Nimba County, Liberia.
The Promoting the Quality of Medicines (PQM) program, funded by the U.S. Agency for International Development and implemented by USP, received financial support from the President’s Malaria Initiative (PMI) and began collaborating with Liberia in 2009 to help build stronger medicines quality assurance systems. The work began with studies assessing the proliferation of poor-quality medicines and helping to draft legislation that established LMHRA. That legislation also allowed LMHRA to create a Quality Control Laboratory (QCL) to test medicines, a Registration Department to ensure registration of imported medicines, and an Inspectorate for post-marketing surveillance of medicines. PQM worked with LMHRA and Liberia’s National Malaria Control Program (NMCP) on the studies to gather post-marketing surveillance data. Reports showed that half of the antimalarial medicine samples from 2010 and 2011 were of poor quality, about two-thirds of which were oral artemisinin-based monotherapy medicines. Also in 2010, the World Health Organization (WHO) called for regulatory action to stop the sale of these monotherapies as one of the main contributing factors to the development and spread of drug-resistant malaria, declaring it “too grave a public health risk.”5 The findings prompted LMHRA to recall failed lots and, in collaboration with NMCP, push for a ban on oral artemisinin-based monotherapies, which was passed in 2011.
LMHRA has expanded its capacity considerably since Liberia and PQM began collaborating, including growing from 3 to 48 staff, improving capacity for key regulatory functions, and obtaining essential laboratory equipment. LMHRA is also working toward ISO 17025:2005 accreditation for its QCL (verification of operating according to international standards), has developed over 65 standard operating procedures, and is continuing to build technical analytical competency. These efforts have helped empower LMHRA to take more than 140 regulatory actions, including the removal of poor-quality and banned antimalarials from the market.
In September 2017, LMHRA and NMCP destroyed 27,600 packs of oral artemisinin-based monotherapies and 143 cartons of other poor-quality medicines confiscated from the 17 districts of Nimba. The products were incinerated by LMHRA, NMCP, and the Environmental Protection Agency of Liberia under the observation of WHO and PQM.
Each enforcement action provides more information to help target resources, so LMHRA can build its capacity for risk-based decision-making. Working with PQM, LMHRA continues to strengthen its ability to find and destroy poor-quality medicines before they reach the people of Liberia.
All listed references were accessed on November 29, 2017.




